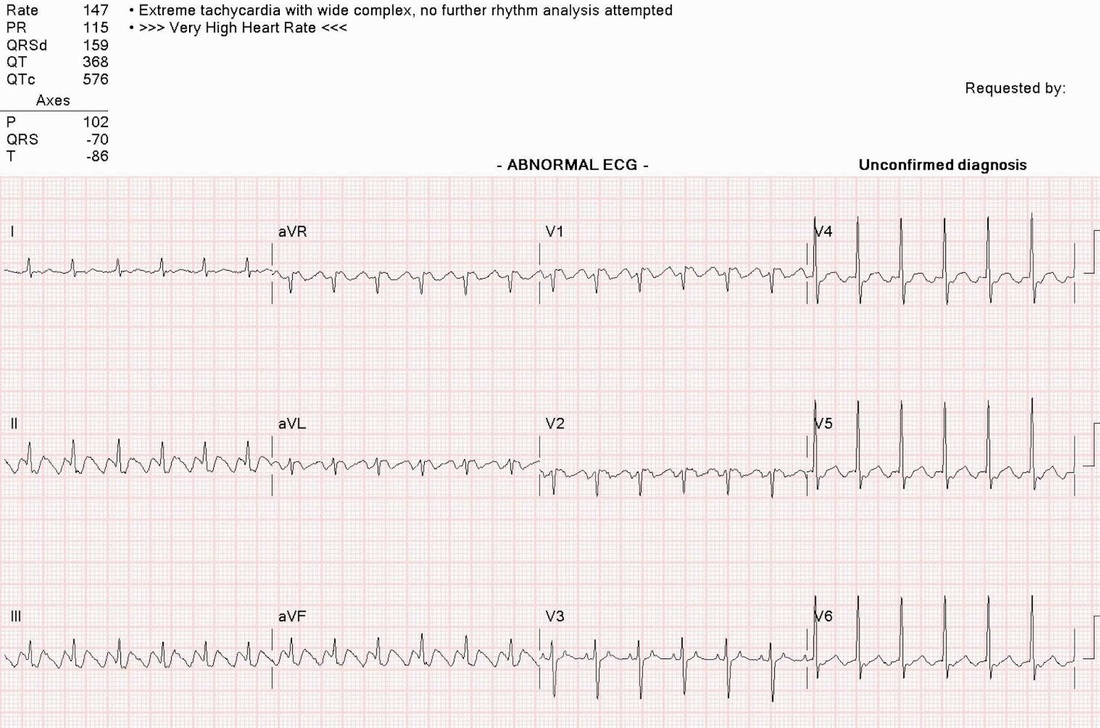
This EKG is a lesson for anyone who simply reads the printed diagnosis at the top of the page and then starts
treating the patient based on that print-out. It says "Extreme tachycardia with wide complex" and ">>>Very High Heart Rate<<<". It's even capitalized. Based on that diagnosis, we probably have a case of ventricular tachycardia and should start antiarrhythmics and applying the cardioversion pads.
That would be a mistake. The monitor couldn't find the real J point (end of the QRS complex) so it mistakenly lists the QRS width at 0.159 seconds. Looking closely at the precordial leads, especially V3, tells a different story. That QRS complex is about 0.08 seconds, well within normal limits. This is some sort of supraventricular tachycardia.
The rate is fast, around 150 beats a minute. The rhythm is highly regular, so its not atrial fibrillation. Your best picture of the supraventricular activity is seen in leads II, III, and AVF. This is atrial flutter with a 2:1 conduction ratio. The AV node is blocking every other flutter wave so the atrial rate of 300 is translated to a ventricular rate of 150. This 2:1 ratio is the most common form of atrial flutter. As a matter of fact, since flutter waves are often hard to see in some leads, you should do a 12 lead EKG on any regular rhythm tachycardia with a rate around 150 so you can look for the characteristic sawtooth baseline in leads II and III. If it's irregular, think atrial fib, however, many regular tachycardias that hold a steady rate near 150 are actually atrial flutter with a 2:1 AV block.
What causes this? It is often seen in conjuction with atrial enlargement. As the atria stretch to unusual size, they may set up a reentry impulse cycle that spins around the atrial, tracing the same electrical path over and over again at ferocious rates (like this one at 300!). If not for the protective blockade provided by the AV node, your patient would have a ventricular rate of 300 also. You wouldn't last long with a heart rate like that.
Remember that our treatment for atrial flutter and atrial fibrillation centers on maintaining an appropriate heart rate, not abolishing the dysrhythmia. Atrial flutter and atrial fibrillation present the danger of thromboemboli if disrupted abruptly. That's why, when you interview these patients, you'll find them taking at least two medications: something for rate control (digitalis, cardizem, verapamil, beta blockers) and something to reduce clotting (warfarin, coumadin).
treating the patient based on that print-out. It says "Extreme tachycardia with wide complex" and ">>>Very High Heart Rate<<<". It's even capitalized. Based on that diagnosis, we probably have a case of ventricular tachycardia and should start antiarrhythmics and applying the cardioversion pads.
That would be a mistake. The monitor couldn't find the real J point (end of the QRS complex) so it mistakenly lists the QRS width at 0.159 seconds. Looking closely at the precordial leads, especially V3, tells a different story. That QRS complex is about 0.08 seconds, well within normal limits. This is some sort of supraventricular tachycardia.
The rate is fast, around 150 beats a minute. The rhythm is highly regular, so its not atrial fibrillation. Your best picture of the supraventricular activity is seen in leads II, III, and AVF. This is atrial flutter with a 2:1 conduction ratio. The AV node is blocking every other flutter wave so the atrial rate of 300 is translated to a ventricular rate of 150. This 2:1 ratio is the most common form of atrial flutter. As a matter of fact, since flutter waves are often hard to see in some leads, you should do a 12 lead EKG on any regular rhythm tachycardia with a rate around 150 so you can look for the characteristic sawtooth baseline in leads II and III. If it's irregular, think atrial fib, however, many regular tachycardias that hold a steady rate near 150 are actually atrial flutter with a 2:1 AV block.
What causes this? It is often seen in conjuction with atrial enlargement. As the atria stretch to unusual size, they may set up a reentry impulse cycle that spins around the atrial, tracing the same electrical path over and over again at ferocious rates (like this one at 300!). If not for the protective blockade provided by the AV node, your patient would have a ventricular rate of 300 also. You wouldn't last long with a heart rate like that.
Remember that our treatment for atrial flutter and atrial fibrillation centers on maintaining an appropriate heart rate, not abolishing the dysrhythmia. Atrial flutter and atrial fibrillation present the danger of thromboemboli if disrupted abruptly. That's why, when you interview these patients, you'll find them taking at least two medications: something for rate control (digitalis, cardizem, verapamil, beta blockers) and something to reduce clotting (warfarin, coumadin).

 RSS Feed
RSS Feed
