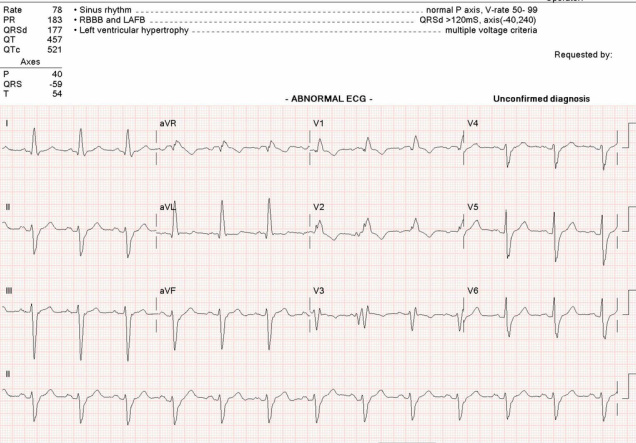
This EKG has lots of interesting stuff in it despite the fact that it is a non-STEMI, sinus rhythm. You will probably first notice the wide QRS complexes and the pathological left axis deviation. These are two distinct issues. One is caused by a bundle branch block, the other by a hemiblock.
Wide QRS Complex
Look at the QRS complex. These are considered wide when they measure greater than 0.10 (2.5 mm) seconds. At 0.12 seconds (3mm) they are pathological. According to the EKG printout, these QRS's are 0.177 seconds wide; they are definitely not normal. Now look at the orientation of the complex in Lead V1. It is mostly positive producing a large R wave. This is an unusual finding because it indicates an electrical vector flowing toward the right side of the heart. In a bundle branch block, the primary electrical flow is toward the blocked ventricle. These QRS complexes indicate a right bundle branch block (RBBB).
Unusual Axis
Now look at the axis. When Lead III is negatively deflected, you have a left axis deviation (LAD). In some cases, this may be a normal finding, a physiological LAD. The way to tell a normal LAD from an abnormal LAD is to check Lead II. If it is also mostly negative, you have a pathological LAD. This patient has inverted Lead II and III complexes, thus has a pathological LAD. Another way to determine pathological LAD is to refer to the hexaxial QRS measurement on the printout. Normal axis is 90 to 0 degrees. Physiological LAD is 0 to about -30 degrees. A pathological LAD is -30 to -90 degrees. This patient has a QRS axis of -59 degrees. The most common reason for a pathological LAD is a left anterior hemiblock. An anterior hemiblock causes a pathological LAD because it throws the ventricular electrical vectors both left and anterior. You can confirm anterior hemiblock with pathological left axis deviation by looking for small R waves in leads II and III.
What the point?
We all have three main conductive paths going down to our ventricles: the right bundle branch, and the two sections of the left bundle branch: anterior and posterior. If you have a block in your right bundle and a block in your left anterior branch, you are running your ventricles off the single, solitary left posterior hemifascicle. This can be a relatively benign and chronic condition or it can be very dangerous. If unsure, the patient should be evaluated for pacemaker placement. In any case, this patient is a single hemifascicle from a complete heart block with enough pathology present to have knocked out the other two paths already.
This is called a bifascicular block because two fascicles or branches are blocked. There are other bifascicular blocks: a RBBB with a posterior hemiblock is relatively rare, but very serious when observed. The other bifascicular block is a LBBB. All LBBB are bifasicular because the LBBB takes down both the anterior and posterior branches of the left bundle. This is why LBBB is clinically more significant than a RBBB.
Left ventricular hypertrophy is indicated because the height of the R waves in AVL is greater than 12 mm.
One more thing about this EKG. Zoom in on the P wave in Lead II. This P wave is 2.5 to 3.0 mm wide and it has a characteristic "M" shape due to the notching of the P wave. This is a mitral P wave or P-mitrale. mitral P waves are a sign of left atrial enlargement. Mitral stenosis is a common cause, thus the name.
Wide QRS Complex
Look at the QRS complex. These are considered wide when they measure greater than 0.10 (2.5 mm) seconds. At 0.12 seconds (3mm) they are pathological. According to the EKG printout, these QRS's are 0.177 seconds wide; they are definitely not normal. Now look at the orientation of the complex in Lead V1. It is mostly positive producing a large R wave. This is an unusual finding because it indicates an electrical vector flowing toward the right side of the heart. In a bundle branch block, the primary electrical flow is toward the blocked ventricle. These QRS complexes indicate a right bundle branch block (RBBB).
Unusual Axis
Now look at the axis. When Lead III is negatively deflected, you have a left axis deviation (LAD). In some cases, this may be a normal finding, a physiological LAD. The way to tell a normal LAD from an abnormal LAD is to check Lead II. If it is also mostly negative, you have a pathological LAD. This patient has inverted Lead II and III complexes, thus has a pathological LAD. Another way to determine pathological LAD is to refer to the hexaxial QRS measurement on the printout. Normal axis is 90 to 0 degrees. Physiological LAD is 0 to about -30 degrees. A pathological LAD is -30 to -90 degrees. This patient has a QRS axis of -59 degrees. The most common reason for a pathological LAD is a left anterior hemiblock. An anterior hemiblock causes a pathological LAD because it throws the ventricular electrical vectors both left and anterior. You can confirm anterior hemiblock with pathological left axis deviation by looking for small R waves in leads II and III.
What the point?
We all have three main conductive paths going down to our ventricles: the right bundle branch, and the two sections of the left bundle branch: anterior and posterior. If you have a block in your right bundle and a block in your left anterior branch, you are running your ventricles off the single, solitary left posterior hemifascicle. This can be a relatively benign and chronic condition or it can be very dangerous. If unsure, the patient should be evaluated for pacemaker placement. In any case, this patient is a single hemifascicle from a complete heart block with enough pathology present to have knocked out the other two paths already.
This is called a bifascicular block because two fascicles or branches are blocked. There are other bifascicular blocks: a RBBB with a posterior hemiblock is relatively rare, but very serious when observed. The other bifascicular block is a LBBB. All LBBB are bifasicular because the LBBB takes down both the anterior and posterior branches of the left bundle. This is why LBBB is clinically more significant than a RBBB.
Left ventricular hypertrophy is indicated because the height of the R waves in AVL is greater than 12 mm.
One more thing about this EKG. Zoom in on the P wave in Lead II. This P wave is 2.5 to 3.0 mm wide and it has a characteristic "M" shape due to the notching of the P wave. This is a mitral P wave or P-mitrale. mitral P waves are a sign of left atrial enlargement. Mitral stenosis is a common cause, thus the name.

 RSS Feed
RSS Feed
